Hepatitis A vaccines are widely available.
Hepatitis A is preventable and, although outbreaks continue to occur in the United States, very few people should ever get infected if preventive measures are taken. For example, food handlers must always wash their hands with soap and water after using the bathroom, changing a diaper, and certainly before preparing food. Food handlers should always wear gloves when handling or preparing ready-to-eat foods, although gloves are not a substitute for good hand washing. Ill food handlers should be excluded from work.
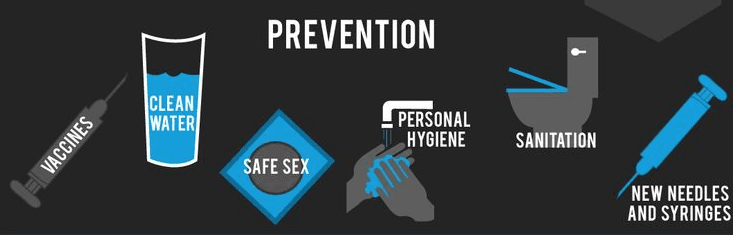
After exposure, a hepatitis A vaccine or immunoglobulin (Ig) can be used to prevent infection. Ig is 90% effective, and the hepatitis A vaccine is 86% effective in preventing clinical hepatitis A when administered within two weeks of the patient’s last exposure. The hepatitis A vaccine is recommended for all people one year old or older to prevent infection after exposure. Ig may also be recommended for those who are immunocompromised or have existing liver disease. Although efficacy is greatest when Ig or the vaccine is administered early in the incubation period, later administration is still likely to make the symptoms of HAV less severe.
In 2006, the ACIP recommended routine hepatitis A vaccination for all children ages 12-23 months, and recommended that hepatitis A vaccination be integrated into the routine childhood vaccination schedule and that children not vaccinated by two years of age be vaccinated subsequently. According to the ACIP, the vaccine is recommended for the following persons:
- People at increased risk for HAV infection
- People traveling to countries at intermediate to high risk for hepatitis A
- Men who have sex with men
- People who use injection or non-injection drugs
- People with occupational risk for exposure
- People who will have close personal contact with a child adopted from outside the U.S.
- People experiencing homelessness
- People at increased risk for severe disease from HAV infection
- People with chronic liver disease
- People with human immunodeficiency virus infection (HIV)
- Other people recommended for vaccination
- Pregnant women at risk for HAV infection
- Pregnant women at risk for severe outcome from HAV infection
- Any person wishing to be vaccinated
Although generally not a legal requirement at this time, vaccination of food handlers would be expected to substantially diminish the incidence of hepatitis A outbreaks.